Categories
Speciality Areas
Myth-busting: pressure mapping is only used to compare cushions

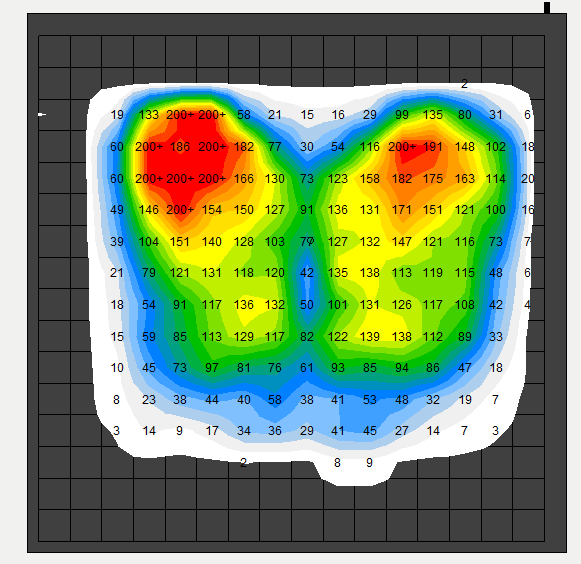
Pressure Mapping as an assessment tool has been in use for more than 30 years, and over that time, the technology has evolved rapidly giving clinicians easy access to routine pressure mapping, as easy as measuring blood pressure. Clinical information accessed from pressure mapping cannot be derived without using the technology which makes it an important tool to support clinical decisions.
As the technology has evolved, mats have become more flexible (easily contours to the shape of the body), data can be accessed in real time, the system has become more cost effective, and the advancements have enabled wireless data sharing.
Pressure mapping as a tool has pre-dominantly been used to compare cushions during clinical assessments to evaluate the dispersing forces applied by a seated person while carrying out the dynamic activity of sitting in real time.
However, pressure mapping has wider applications.
Pressure mapping can be used to visualise whether the pressure has been redistributed as a result of any seat or positioning adjustment. Back in the 90s, Professor Ian Swain reported, that the simplest way to get better redistribution of pressures away from the boney areas of the pelvis (ITs), was to adjust the position of the foot support. Height adjustments to the foot support would result in more pressure distributed under the thighs.
Pressure imaging allows you to see the optimum set up of the different parts of the chair – foot supports, arm supports, back support, etc., from which clinical decisions can be made to adjust these support to deliver optimal pressure redistribution.
It can also be an excellent educational tool for both users and carers. The technology, through colourful images, shows the effects of good and bad positioning. It is a great tool to show how far the far user needs to offload their ITs to get better pressure distribution.
In recent years, the greater impact of shear strain on tissues/skin integrity, rather than pressure alone, has become more widely known. Using the ‘gradiant view’ within a pressure mapping system, allows the clinician to visualise the greatest rate of change in pressure (the greater the pressure gradient, the greater chance of distortion of the skin tissues.
Even though pressure mapping systems are less expensive, the question of justifying ‘how a pressure mapping system can pay for itself’, always comes up when budgets are concerned. Apart from the clinical outcomes, pressure mapping systems can collate information and document the effects of different solutions assessed in a clinic. This can be used as the justification for the best solution prescribed. Using it as a support and evidence tool also reduces the risks poor equipment supply or incorrect judgement, which could in turn lead to litigation.
Hence, Pressure Mapping Systems can be a very useful tool for clinicians, carers, users and healthcare facilities to help make appropriate clinical decisions, and provide the right solution for the user.