Categories
Speciality Areas
What makes a good trunk support? Part 6: Postural variation

Different postures are required for different activities. In this part we review the impacts that different postures have on the seated occupant, and the impact that adjustments to their seating system can have on the occupant’s functionality.
Sitting is an activity, and postures will change during the day to accommodate for fatigue, changes in tone, etc, in addition to the changes needed to achieve functional activities. Functional movements during wheelchair use such as head and upper extremity movements are most effectively executed when multiple body segments are involved, so we need to be able to vary our postures to achieve our required outcomes.
Adjusting the position of one part of the body frequently has an impact on at least one other part of the body, often a good distance apart. When you look up to the ceiling when seated, you will need to extend your neck, i.e. your cervical spine – but extending the neck can also be assisted by some extension of the thoracic or even lumbar and pelvic segments. Conversely, changes in your foot position may have an impact on your head’s position.
Other impacts can occur from proximal changes such as reclining the back support or tilting the seating system, where even a small change can have a large impact on the effectiveness, or even safety, of various seating accessories.
Tilt in space
Tilt in space has often been recommended as a means to reduce the pressures on the occupant’s ischial tuberosities, the bony parts on the base of the pelvis, but to achieve this the seating system needs to be lilted back at least 30 degrees: this may be a great position to relax in, but otherwise is not very functional. With tilt in space, the orientation of the seating system components that are attached to the seating system (as compared with being attached to the frame of the wheelchair) and therefore sections of the body, stay fixed, but the orientation of the whole body changes.
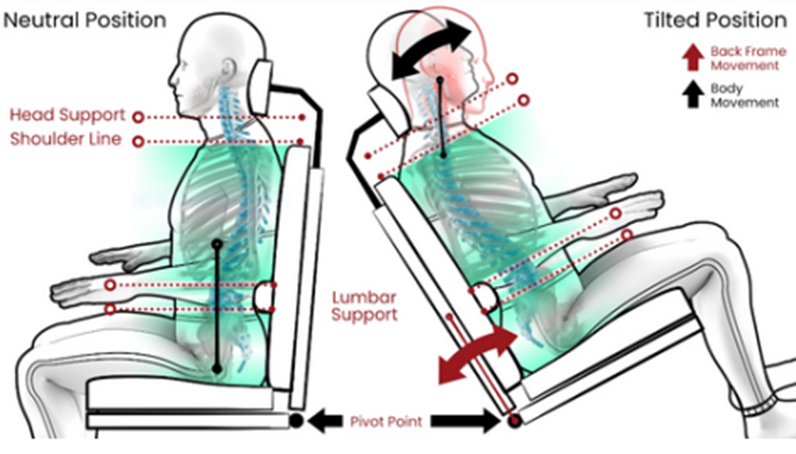
The part of the body that tends to be affected most is the head since the occupant is left staring at the ceiling initially. To be able to react with their surroundings they then make postural adjustments, such as flexing their neck to adjust their line of sight (Figure 1). This can lead to greater trunk flexion into the back support which in turn can result in the pelvis being pushed forward. Ultimately the occupant will probably need an assistant to help them reposition themselves.
Recline
A common postural adjustment device on a seating system will be the recline function. This is where the most frequent problems occur: the fulcrum point for the device is usually at the junction between the back support and the seat – which is not level with the fulcrum of recline in the occupant’s body, which is the hip joint (Figure 2). The result is that during recline there are shear forces between the occupant’s back and the seat’s back support as the two move different amounts relative to each other. At the same time accessories attached to the back support, such as lateral or head supports, will move up the trunk and out of position relative to the part of the body they are supposed to be supporting. In addition, with the pelvis being rotated into a greater posterior tilt, there is a risk of the occupant sliding forward on their seat, thereby also adding frictional and shear forces under the buttocks.
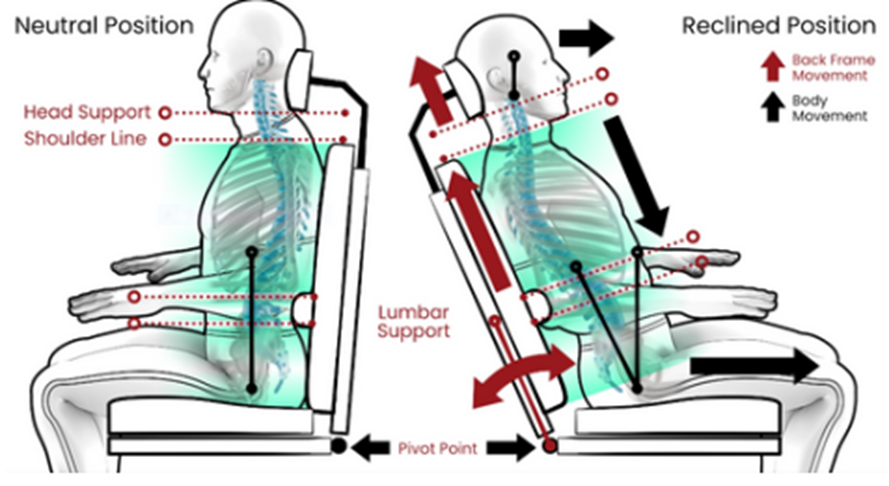
In the past, the shear forces on the occupant’s back have been addressed by the back support material being on rollers and allowed to move with the occupant’s body, but this did not address the positioning challenges. Biangular back supports allow for just static separation of the pelvis from the trunk. Recently an innovative approach has been made available in the EPiC seating system, which allows for dynamic separation of these two parts of the posterior support, where the recline pivot point is aligned with the body’s pivot point of the hip joint (Figure 3).
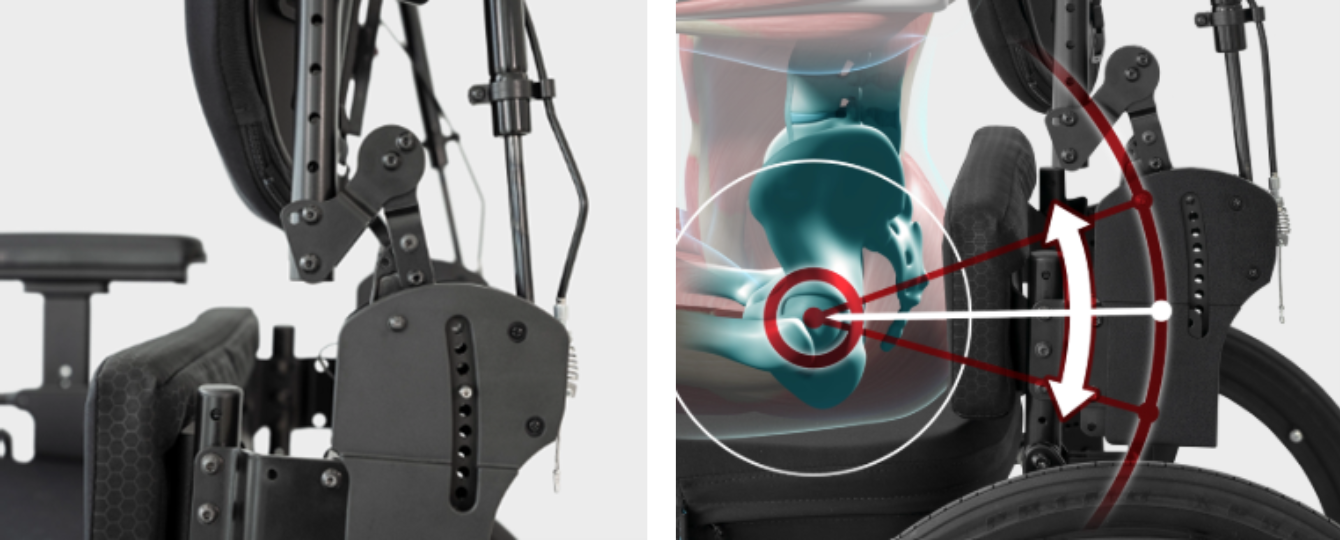
The result is that while the pelvis to thigh angle is maintained, the lower and mid-thoracic areas can move backwards. The lumbar spine will follow and extend without direct force on the stiff lumbar spine. This innovative approach and movement enables spine extension with minimal shear and friction at the occupant- back support interface and the occupant-seat cushion interface.
Since the movement of the thoracic spine occurs in sync with the occupant’s movements there are no shifts in the attached PSDs such as head supports or lateral supports, when this movement occurs. In addition the position of the thoracic spine is crucial for obtaining a functional head position and upper extremity function and helps to reduce the amount of energy needed from postural muscles to sit upright.
There’s three optional methods for use:
- Adjusting, then maintaining an appropriate pelvis to thigh angle for the occupant. This can also be used where the occupant has a hyperkyphotic spine to relieve the degree of neck hyperextension needed to achieve a functional eyeline.
- Caregiver induced passive postural variation, by allowing the lower and mid-thoracic segments of the back support to move backward (which can be symmetrical or asymmetrical) in sync with the movement of the spine (Figure 4).
- Occupant induced active postural variation (arising from postural fatigue, upper extremity movements, or tone, for example) causing the lower and mid- thoracic segments to move backwards (symmetrically or asymmetrically), in sync with the movements of the spine, and the gas struts then assist a return into a more neutral resting position as desired.

Upper body extremities
The back support is the usual mounting point for the head support: aspects to be considered around this have been covered in the “What makes a good head support?” articles in this series.
What about the relationship of the trunk support to the shoulder girdle, arms, and hands? As discussed in Part 5, most wheelchair occupants do not need a back support any higher than being level with the base of the scapulae, because there is normally no contact between the occupant’s back and back support above this point (an exception is occupants undergoing high tone extensor spasms, for example). Indeed, a higher-positioned back support will impair the occupant’s range of upper body movement, and therefore their functionality.
Of great importance for most people’s functionality is the use of their hands, whether for writing, eating, texting, or operating a joystick, for example. An appropriately positioned back support can facilitate this functionality, but on top of this is the back support’s physical relationship with the chair’s arm supports. This is where there has been a tendency towards inappropriate design.
For most people the anatomically correct, and therefore comfortable position, is to have our hands in front of us, and not rotated outwards along a chair’s standard arm supports. The result is that maybe our elbows alone are placed on these supports, and frequently these are not at the appropriate height to support the upper arm correctly in the shoulder socket. Without proper support at this point, occupants (particularly those with reduced joint proprioceptive sensation after, for example, a stroke) end up with subluxed joints and consequent extreme pain. This all could be prevented by early intervention with an appropriately positioned arm support.
One such support is Bodypoint’s Dynamic Arm Support (DAS) (Figure 5) which was invented by the renowned Belgian physiotherapist, Bart Van der Heyden (also the inventor of the EPiC seating system!). The DAS provides three points of support – at the elbow, along the forearm, and at the hand, with all parts designed to provide anatomically correct heights and angles of support and movement.

The clinical benefits and outcomes include:
- Contracture prevention and management
- Reduction of shoulder pain
- Mitigated impact of abnormal upper extremity tone
- Strength and proprioceptive training of the upper extremity
- Prevent and minimize shoulder subluxation
- Minimise injury to the upper extremity
However, the DAS will only be effective if the positioning of the arm and hand are set up correctly for the occupant, and that any postural variation around the seating system does not affect this set-up. This is equally true in relation to all other functional uses of the hands where upper body positioning is crucial.
In conclusion
A good trunk support correctly prescribed and positioned can keep the occupant safe, and can facilitate daily functional activities. Sitting is an activity and involves frequent postural variation. It is important that the elements of the seating system facilitate this variation in a safe and effective way.